Agitation means that a person is restless and worried. He or she doesn't seem to be able to settle down. Agitated people may pace a lot, not be able to sleep, or act aggressively toward others. They may verbally lash out or try to hit or hurt someone. Most of the time, these behaviors happen for a reason. When they happen, try to find the cause.
For example, the person may have:
- Pain, depression, or stress and not know how to explain it
- Too little rest or sleep
- Constipation
- Soiled underwear or diaper
- Sudden change in a well-known place, routine, or person
- • A feeling of loss. For example, the person with Alzheimer's Disease may miss the freedom to drive or the chance to care for children
- Too much noise or confusion or too many people in the room
- Being pushed by others to do something. For example, to bathe, or remember events or people, when Alzheimer's Disease has made the activity very hard or impossible
- Feeling lonely and not having enough contact with other people
- Interaction of medicines
- Look for the early signs of agitation or aggression. If you see the signs, you can deal with the cause before the problem behaviors start.
- Try not to ignore the problem. Doing nothing can make things worse. Try to find the causes of the behavior. If you deal with the causes, the behavior may stop.
- Slow down and try to relax if you think your own worries may be affecting the person with Alzheimer's Disease. Try to find a way to take a break from caregiving.
- Allow the person to keep as much control in his or her life as possible.
- Try to distract the person with a favorite snack, object, or activity.
- Reassure him or her. Speak calmly. Listen to the person's concerns and frustrations. Try to show that you understand if the person is angry or fearful.
- Keep well-loved objects and photographs around the house. This can make the person feel more secure.
- Reduce noise, clutter, or the number of people in the room.
- Try gentle touching, soothing music, reading, or walks.
- Build quiet times into the day, along with activities.
- Limit the amount of caffeine, sugar, and "junk food" the person drinks and eats.
- Give the person a medical exam to find any problems that may cause the behavior. These problems might include pain, depression, or the effects of certain medicines.
- Check the person's vision and hearing each year.
- Protect yourself and your family members from aggressive behavior. If you have to, stay at a safe distance from the person until the behavior stops.
- As much as possible, protect the person from hurting himself or herself.
- Ask the doctor or Alzheimer's Disease specialist if medicine may be needed to prevent or reduce agitation or aggression.
_____________________________
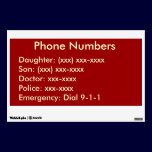
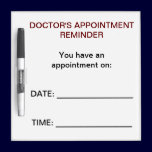
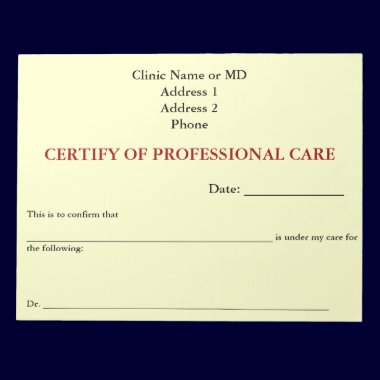
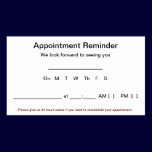
Caregiving Tools
$35.95 - Reminders Dry Erase Board