Suggestions
- Identify, within the organization, a motivated employee who possesses leadership skills and is willing to take on the responsibility for training staff in the assessment of balance problems. Provide this staff member with additional training on the assessment of balance problems so he/she becomes the in-house trainer and expert. With proper fall prevention training, this person will also be able to develop fall prevention plans for identified fall risk patients and analyze falls after they occur.
- Train all new staff members on the organization's balance assessment tool. Repeat this training as part of your organization's annual staff training program and document attendance in each employee's file. Schedule training sessions with the in-house trainer for any new staff who will be directly responsible for conducting balance problem assessments. Have both the new staff member and an experienced staff member assess several patients independently and then compare scores and discuss outcomes.
- Request that the in-house trainer complete a "report card" or performance review of all new employees who are trained in the assessment of balance problems. Maintain these records as part of each employee's personnel file.
- Teach new staff to assess environmental living conditions first for anything that may contribute to the patient's balance problem, such as loose carpeting or floorboards, scatter rugs, clutter or stairs. Have them consider what changes could be made to improve the safety of the environment, such as extra stair railings, grab bars in the bathroom and a raised toilet seat.
- Train staff to observe the patient for any physical deformities or conditions that might impact his/her balance, such as tremors, lower leg edema or signs of pain. Pain medication, diuretics and blood pressure control medications can also impact balance. Ask the staff to discuss any other health conditions, eg., neurological or psychiatric, that might contribute to falling.
- Ask the staff to check patients' footwear for excessive wear on the soles, any bending or caving in of the shoe at the ankle which may indicate a gait or walking-style problem. Remind the staff of the additional foot and shoe issues faced by the diabetic patient. Diabetics are very susceptible to circulation problems and infection. Tight shoes can constrict circulation and lead to diabetic foot wounds that can impact patients' walking ability and balance.
- Train staff to assess motor strength and skills. Ask staff to check for range of motion in a patient's extremities. Ask the patient to stand from a chair and check for steadiness within the first five seconds. Check for steadiness as the patient stands with feet together and eyes closed. Have staff stand by the patient to prevent any falls.
- Teach the staff to assess for walking ability and gait. Train them to measure the length and the height of the step along with the symmetry of the steps. Normal gait should have equal length and height of steps; limping or dragging a foot or leg will cause an unequal length and height of the step. "Symmetry of the steps" means the patient's walking pattern shows equal-sized steps. Any foot or leg pain will cause a shortening of steps on that side of the body. Teach the staff how to discern whether the patient's walking stance is within "normal" and have them determine whether the patient can walk in a straight line. Have staff observe the patient doing the "touch the nose" test by having him/her touch finger to nose while standing, with eyes closed.
Tips
- The specific balance tests you conduct will depend on your organization's balance assessment protocol. Each assessment tool will have a score affixed to each activity. Once the balance assessment tool has been scored, staff will share the results with the patient's physician, the nursing staff and any other caregivers. Be sure to document the results in the patient's chart.
- Take precautions so the patient does not fall during the balance assessment process.
_____________________________
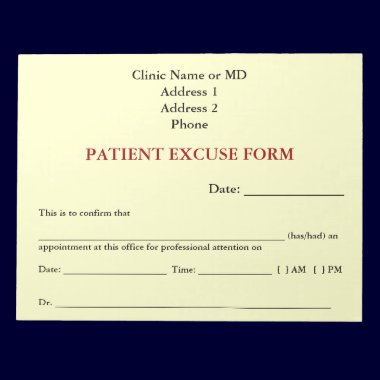
For Your Practice
$4.50 - Thank You Note Cards
see on 2 styles

















No comments:
Post a Comment